Mesh Complications Patient Story 45
Right & Left lower Abdominal Pain, Vaginal Pain, Vaginal Discharge, & Mesh Extrusion following a Sacral Colpopexy
Mesh Complications: Right and left lower abdominal pain, vaginal pain, brown vaginal discharge, vaginal pressure and suspected recurrent prolapse
Treatment: Laparoscopic removal of the sacral colpopexy mesh
This patient is a 47-year-old female with complaints listed above. She claims her problems started after a sacral colpocervicopexy and a paravaginal repair for uterine prolapse and a cystocele utilizing PelvitexT (Polypropylene Mesh, CR Bard). She had the surgery five years ago. The patient reports in 2010, she had a mesh extrusion through the vaginal skin. The surgeon trimmed the mesh in the office. One year later she began to have brown vaginal discharge. She went back to her original urogynecologist located at a large university hospital in Boston. Reportedly, the surgeon told her there was “something there” and it would be a minor surgery. She asked if she had uterine prolapse and she was told that the uterus was well supported by the previous surgery.
The patient is a resident of Maine and decided to fly to Atlanta for evaluation by Drs. Miklos and Moore for possible removal of the entire mesh. Examination revealed a half dollar size mesh extruding through the apex of the vagina. More importantly, the patient’s uterus had prolapsed, and her cervix was at the opening of the vagina. Her surgeon in Boston had examined her only two months earlier and told her that her uterus was well supported. Dr. Miklos confirmed the patient’s suspicions, the mesh had eroded through the vaginal skin, and the sacral colpopexy had failed to keep the uterus supported.
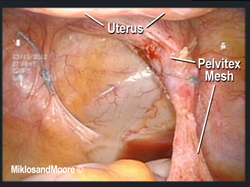
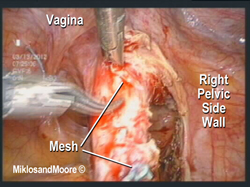
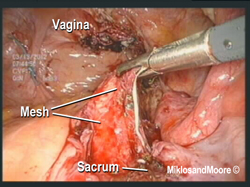
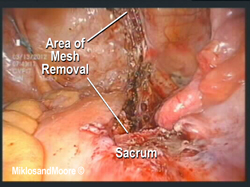
The patient was taken to the operating room the next day and a laparoscopic approach was utilized (i.e. mini incisions) (Figure 1) to identify (Figure 2) the mesh, and dissect it away from the right pelvic sidewall (Figure3).
Picture 1 & 2- The previously placed mesh is identified in the pelvis. There did not appear to be any infection present in the upper pelvis (i.e. the upper portion of the mesh did not appear to be infected and had healed in place) and it did not appear that the infection had tracked its way up the mesh from where it was infected on the vaginal attachment.
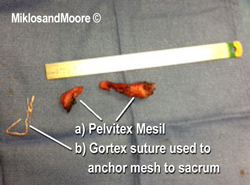
After freeing the mesh it was detached from the points of attachment at the vagina (Figure 4) and from the sacrum (Figure 5).
Dr. Miklos Comments: This patient has a long history of uterine prolapse and had a uterine suspension (using her original uterosacral ligaments) seven years ago. Then five years ago had the sacral colpopexy in Boston, MA. Neither surgery worked. The patient elected to remove mesh and suspend her uterus using natural ligaments.
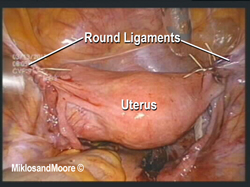
Upon removal of the mesh, the defect left behind in the vaginal skin was removed, and the hole was closed with suture. The uterus was suspended without mesh as requested by the patient. The uterus was suspended by suturing her uterus to her uterosacral ligaments and by shortening her round ligaments (Figure 6 **Uterosacral ligaments not visible. Her uterus obstructs them).
Post- operatively the patient almost immediately noted the resolution of her pain. The mesh was almost completely removed approximately 95%, and the patient remains happy with the results of the surgery.